Cytology is the examination of cells collected from body fluids, fine needle aspiration (FNA), or impression smears from solid tissue lesions. It is a relatively non-invasive technique with the added advantage of requiring no or minimal sedation in the majority of patients. The turnaround time is more rapid than that for histopathology, with results generally available within one working day. With good sample quality (i.e., adequate numbers of intact cells that are well spread out), clinical description and history, cytology can provide a definitive diagnosis or give useful information with regard to further testing modalities, or treatment options.
Sites and tissues well suited to cytological examination include:
- Cutaneous and subcutaneous masses – Masses of spindle cell origin (i.e., sarcomas) are generally less exfoliative than round cell or epithelial masses and architecture is required to differentiate subtypes
- Nasal cavity samples and masses
- Bronchial and tracheal washes
- External ear canal
- Lymph nodes
- Synovial fluid
- Pleural, pericardial and peritoneal fluids
- CSF taps – Being mindful that if the lesion is caudal to the cisterna magna, then a lumbosacral puncture is recommended. Cells are very fragile, and special handling is recommended (see below)
- Prostatic aspirates/washes
- Vaginal and uterine smears
- Blood smears
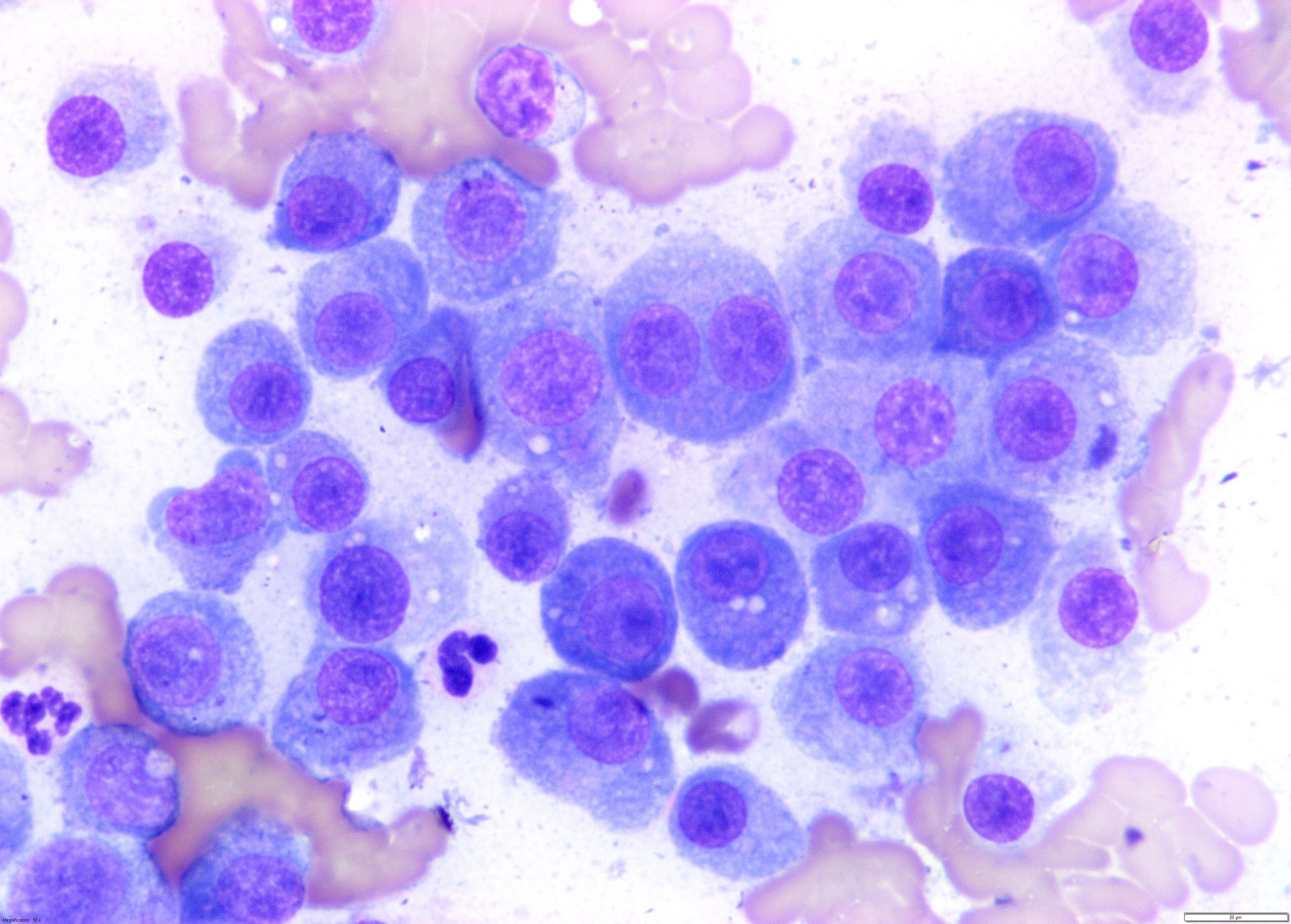
- Bone marrow
- Liver – Diffuse processes (e.g., infiltrative tumours, fatty changes) have a higher diagnostic yield than solitary masses (these may even be difficult to diagnose on histology)
- Intra-abdominal / thoracic masses – Ultrasound guided generally gives better result
- Urine / masses in the urinary bladder
- Spleen – Non-aspiration technique may be best
Sites less well suited to cytological examination, requiring greater attention to sample collection technique, or absolutely requiring biopsy for diagnosis of malignant potential:
- Kidney – Blood filled organ, unless a diffuse process is present (e.g., lymphoma), these samples are often non-diagnostic
- Mammary gland – specifically in canine, histology is preferable. Cytology can confirm a mass of mammary epithelial origin (rather than lipoma or mast cell tumour, for example). However, histopathology is required to confirm malignancy in dogs (because invasion cannot be assessed by cytology). In cats, cytology can be helpful as the majority of feline mammary neoplasms are malignant
- Lung – Often unrewarding because it is a blood filled organ, although FNA of distinct mass lesions may be diagnostic.
- Skin tumours on nose / ear tips (e.g., squamous cell carcinoma) – FNA if possible, or deep scrapings as impression smears often reflect only surface inflammation and dysplastic epithelium
- Oral masses – FNA preferred as impression smears often reflect only surface inflammation and dysplastic epithelium
- Conjunctival scrapes – If not deep enough or not enough material on slide, these samples can be non-diagnostic. Using a cytobrush on the lesion and gently rolled onto the slide can work very well.
- Rectal mucosal scrapes
- Firm fibrous masses – Architecture is often an absolute requirement for determining whether these are scar tissue, the edge of a cyst, granulation tissue, or a neoplasm. If the latter, which specific subtype of mesenchymal neoplasm. Therefore, incisional / excisional biopsy will often be required. If that is not possible, then multiple needle passes or aspiration technique may assist cell exfoliation.
- Cystic/fluid filled skin lesions – May be cell-poor and therefore not have enough cells to permit a diagnosis. Aiming for the wall of the cyst in addition to the centre may help. However, incisional or excisional biopsy is generally required because architecture is the key to understanding many of these cystic processes.
Things to avoid:
- Exposure of cytological material to formalin – including close exposure in the operating theatre, or being packaged in the same bag as the formalin-filled pottle. Formalin fumes prevent cellular uptake of differential stains rendering the slides non-diagnostic. Wrap cytology smears separately from histology containers and place in different plastic bags.
- Sufficiently dried smears should be placed in clean, dry slide holders – Do not use flame or heat fixation – rapid air drying (ideally with a fan, or vigorous arm flapping) is sufficient
- Do not refrigerate smears at any time – The cells will lyse when condensation forms on the slide after removal from the fridge
- Fluids however, should be refrigerated (never frozen) if there is a delay in dispatch. Make a smear of fluids prior to refrigeration.
- Urine should be refrigerated (never frozen) if there is a delay in dispatch.
- CSF should be processed within 4 hours of collection. If this is not possible, then adding autologous serum will help preserve cellular integrity (EDTA alone does not do this). For example, if there is approximately 90uL of CSF, then add 10uL of serum (2-3 drops; see below).